AMD ( age related macular degeneration) is a condition that occurs when cells in the macula degenerate. Damage to the macula affects your central vision which is needed for reading, writing, driving, recognizing people’s faces and doing other fine tasks. This loss of central vision will severely affect normal sight.
AMD can affect anyone. It becomes more common with increasing age. If you develop AMD in one eye, you have a high chance (about 6 in 10) that it will also develop in the other eye. About 5 in 100 people aged over 65 have AMD severe enough to cause serious visual loss.
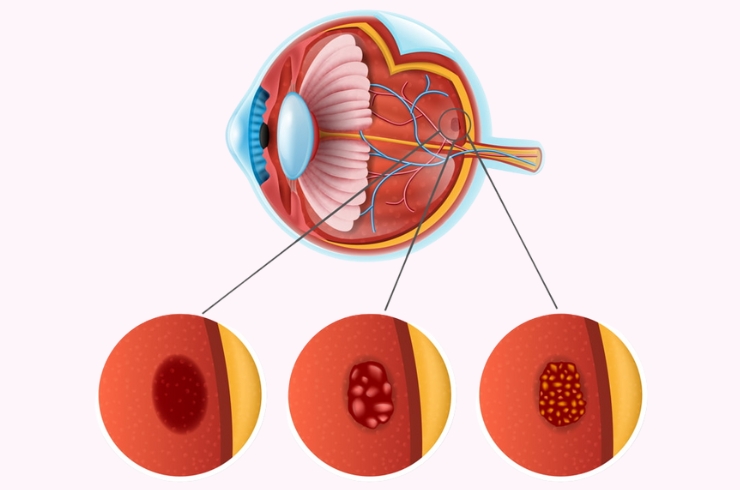
This is the most common form. In this type the cells in the RPE of the macula gradually become thin, degenerate and dry. This layer of cells is crucial for the function of the rods and cones which then also degenerate and die. Typically, dry AMD is a very gradual process and usually takes several years for vision to become seriously affected.
Wet AMD may also be called neovascular or exudative AMD. It occurs in about 1 in 10 cases. However, it is likely to cause severe and sudden visual loss over quite a short time – sometimes just months. In wet AMD, in addition to the retinal pigment cells degenerating, new tiny blood vessels grow from the tiny blood vessels in the choroid. This is called choroidal neovascularisation. These vessels are not normal. They are fragile and tend to leak blood and fluid. This can damage the rods and cones, and cause scarring in the macula, causing further vision loss.
In people with AMD the cells of the RPE do not work so well with advancing age. They gradually fail to take enough nutrients to the rods and cones, and do not clear waste materials and byproducts made by the rods and cones either. As a result, tiny abnormal deposits called drusen develop under the retina. In time, the retinal pigment cells and their nearby rods and cones degenerate, stop working and die. Sometimes it also triggers new blood vessels to develop from the choroid.
The main early symptom is blurring of central vision despite using your usual glasses.
The ophthalmologist will examine the back of your eye with a slit lamp microscope to evaluate your retina.
OCT is done to get very detailed ‘3D’ information about the macula. It is also a useful test to assess and monitor the results of any treatment.
FFA (fluorescein angiography) is done in which a dye is injected into a vein in your arm. Then, by taking pictures with a special camera, the ophthalmologist can see where any dye leaks into the macula from the abnormal leaky blood vessels. This test can give an indication of the extent and severity of the condition.
In recent years a group of medicines called anti-VEGFs has been developed. Vascular endothelial growth factor is a chemical that is involved in the formation of new blood vessels in the macula in people with wet AMD. By blocking the action of this chemical, it helps to prevent the formation of the abnormal blood vessels that occur in wet AMD. Avastin and Lucentis are two such injections.
The anti-VEGF medicines are injected using a fine needle directly into the vitreous of the eye. Repeat Anti VEGF injections are needed every four weeks. A loading dose of 3 injections given a months interval is used followed by additional injections if required. On average a patient would require about 5-6 injections per year
A medicine called verteporfin is injected into a vein in the arm. Within a few minutes the verteporfin binds to proteins in the newly formed abnormal blood vessels in the macula. A light at a special wavelength is then shone into the eye for just over a minute which activates verteporfin and causes damage, destroying the abnormally growing blood vessels (neither damaging the nearby rods and cones, nor any normal blood vessels). Success means that the visual loss is prevented from getting worse – it does not restore any lost vision. Treatment usually needs to be repeated every few months to continue to suppress newly growing blood vessels. The main advantage that this method has is less damage to the normal retina.
When your vision becomes poor, it is common to be referred (by your ophthalmologist) to a low vision clinic. Staff at the clinic provide practical help and advice on how to cope with poor and/or deteriorating vision.